Overview of Cancer: What You Need to Know
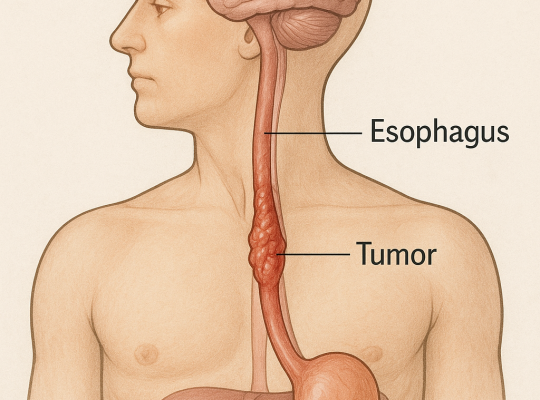
Cancer, a complex and multifaceted disease, affects millions of individuals globally each year. It arises when abnormal cells in the body grow uncontrollably, forming malignant tumors that can invade nearby tissues and spread to other parts of the body through the bloodstream or lymphatic system. There are over 100 different types of cancer, each with its own unique characteristics and behavior. Despite its prevalence, considerable strides have been made in understanding the biology of cancer, leading to improved diagnostic techniques and more effective treatments.
The process of cancer development, or carcinogenesis, typically involves a series of genetic mutations that disrupt normal cell growth and division. These genetic changes can be inherited, caused by environmental factors such as exposure to carcinogens, or occur spontaneously. Researchers continue to investigate the intricate mechanisms behind these mutations, seeking to uncover new targets for intervention and therapy. Advances in molecular biology and genomics have been instrumental in identifying the specific genetic alterations that drive various forms of cancer.
While the diagnosis of cancer can be devastating, it is important to recognize that significant progress has been made in cancer care. Survival rates for many types of cancer have improved dramatically over the past few decades, thanks to early detection, better treatment options, and advancements in supportive care. By staying informed about the latest research and treatment developments, patients and their families can make empowered decisions and remain hopeful in their journey against cancer.
Recent Advances in Cancer Research
In the realm of cancer research, the past few years have been marked by remarkable discoveries and technological innovations. One of the most promising areas of research is the field of genomics, which involves studying the complete set of genetic material in cancer cells. By sequencing the genomes of tumors, scientists can identify specific mutations and genetic alterations that drive cancer progression. This knowledge has paved the way for the development of targeted therapies, which aim to inhibit the activity of these mutations and halt tumor growth.
Another significant breakthrough in cancer research is the advent of liquid biopsies. Traditional biopsy methods require the removal of a tissue sample from the tumor, which can be invasive and sometimes risky. Liquid biopsies, on the other hand, analyze circulating tumor DNA (ctDNA) found in a patient’s blood. This non-invasive technique allows for the detection of genetic mutations and monitoring of treatment response in real time. Liquid biopsies have the potential to revolutionize cancer diagnostics and personalized treatment plans.
Additionally, the exploration of the tumor microenvironment has provided new insights into cancer biology. The tumor microenvironment consists of various cells, molecules, and blood vessels that surround and interact with the tumor. Understanding how these components influence tumor growth and metastasis has led to the identification of novel therapeutic targets. For example, researchers have discovered that certain immune cells within the microenvironment can either promote or inhibit cancer progression. By modulating these immune cells, scientists are developing innovative strategies to enhance the body’s natural defense mechanisms against cancer.
Innovative Treatment Options: A Closer Look
Innovative treatment options for cancer are continually emerging, offering new hope for patients. One such approach is targeted therapy, which involves using drugs or other substances to specifically target and inhibit the activity of cancer-causing genes or proteins. Unlike traditional chemotherapy, which can affect both cancerous and healthy cells, targeted therapy aims to minimize damage to normal tissues. This precision medicine approach has shown remarkable success in treating certain types of cancer, such as breast cancer, lung cancer, and melanoma.
Another groundbreaking treatment option is CAR-T cell therapy, a form of immunotherapy that harnesses the power of a patient’s own immune cells to fight cancer. In CAR-T cell therapy, T cells are extracted from the patient’s blood and genetically modified to express chimeric antigen receptors (CARs) that recognize and attack cancer cells. These engineered T cells are then infused back into the patient, where they seek out and destroy cancerous cells. CAR-T cell therapy has shown remarkable efficacy in treating certain types of blood cancers, such as leukemia and lymphoma.
Furthermore, advances in radiation therapy have led to the development of more precise and effective techniques. Stereotactic body radiation therapy (SBRT) and proton therapy are two examples of cutting-edge radiation treatments that deliver high doses of radiation directly to the tumor while sparing surrounding healthy tissues. These techniques allow for more accurate targeting of cancer cells, resulting in improved outcomes and reduced side effects for patients. As technology continues to evolve, radiation therapy is becoming an increasingly powerful tool in the fight against cancer.
The Role of Immunotherapy in Cancer Treatment
Immunotherapy has emerged as a revolutionary approach in cancer treatment, leveraging the body’s own immune system to combat the disease. Unlike traditional treatments that directly target cancer cells, immunotherapy works by enhancing the immune system’s ability to recognize and destroy cancerous cells. This innovative strategy has shown remarkable success in treating various types of cancer and has become a cornerstone of modern oncology.
One of the most well-known forms of immunotherapy is immune checkpoint inhibitors. These drugs work by blocking proteins on immune cells, such as PD-1 and CTLA-4, that act as brakes on the immune response. By inhibiting these checkpoints, the immune system is unleashed to attack cancer cells more effectively. Immune checkpoint inhibitors have demonstrated significant efficacy in treating melanoma, lung cancer, and other malignancies. Their success has led to the approval of several checkpoint inhibitors for clinical use, offering new hope to patients who previously had limited treatment options.
Another promising avenue of immunotherapy is cancer vaccines. Unlike traditional vaccines that prevent infectious diseases, cancer vaccines are designed to stimulate the immune system to target and eliminate cancer cells. These vaccines can be made from tumor antigens, which are proteins expressed by cancer cells, or from the patient’s own tumor cells. By training the immune system to recognize and attack these antigens, cancer vaccines hold the potential to prevent cancer recurrence and improve patient outcomes. Ongoing research and clinical trials are exploring the efficacy of various cancer vaccines in different types of cancer.
Moreover, adoptive cell transfer (ACT) is a cutting-edge immunotherapy technique that involves extracting immune cells from a patient, modifying or expanding them in the laboratory, and then reinfusing them back into the patient to fight cancer. CAR-T cell therapy, mentioned earlier, is a form of ACT that has shown remarkable success in treating blood cancers. Other forms of ACT, such as tumor-infiltrating lymphocyte (TIL) therapy, are also being investigated for their potential to treat solid tumors. The field of immunotherapy continues to evolve, with ongoing research aimed at enhancing its efficacy and expanding its applications to benefit more patients.
Personalized Medicine: Tailoring Treatment to Individual Patients
Personalized medicine, also known as precision medicine, is an approach that tailors medical treatment to the individual characteristics of each patient. In the context of cancer, personalized medicine involves understanding the unique genetic and molecular profile of a patient’s tumor to design a customized treatment plan. This approach has revolutionized cancer care, offering more effective and targeted therapies with fewer side effects.
One of the key components of personalized medicine is genomic profiling. By analyzing the genetic mutations and alterations in a patient’s tumor, oncologists can identify specific targets for treatment. For example, certain mutations in the EGFR gene are known to drive the growth of non-small cell lung cancer. Targeted therapies that inhibit EGFR activity have shown remarkable efficacy in treating patients with these mutations. Genomic profiling allows for the identification of such actionable mutations, enabling the selection of the most appropriate targeted therapy for each patient.
Furthermore, personalized medicine extends beyond genetic profiling to include other biomarkers, such as protein expression and immune markers. For instance, the presence of the HER2 protein in breast cancer tumors can predict the response to HER2-targeted therapies like trastuzumab. Similarly, the expression of PD-L1 on tumor cells can indicate the likelihood of response to immune checkpoint inhibitors. By integrating these biomarkers into treatment decisions, personalized medicine aims to optimize therapy and improve patient outcomes.
In addition to selecting targeted therapies, personalized medicine also encompasses the use of advanced diagnostic tools and monitoring techniques. Liquid biopsies, mentioned earlier, play a crucial role in personalized medicine by providing real-time insights into the genetic landscape of a patient’s tumor. This non-invasive approach allows for continuous monitoring of treatment response and detection of emerging resistance mutations. By adapting treatment strategies based on these insights, personalized medicine aims to stay one step ahead of the evolving cancer and provide the best possible care for patients.
The Importance of Early Detection and Screening
Early detection and screening are critical components of effective cancer management. Detecting cancer at an early stage, when it is most treatable, significantly improves the chances of successful treatment and long-term survival. Regular screening and vigilant monitoring can identify precancerous conditions and early-stage cancers before they progress to more advanced and difficult-to-treat stages.
Screening methods vary depending on the type of cancer. For example, mammograms are commonly used to screen for breast cancer, while colonoscopies are used to detect colorectal cancer. Pap smears and HPV testing are essential for cervical cancer screening, and low-dose CT scans are recommended for lung cancer screening in high-risk individuals. These screening tests have been proven to reduce cancer-related mortality by enabling early intervention and timely treatment.
In addition to traditional screening methods, advances in imaging technology and molecular diagnostics have enhanced the accuracy and sensitivity of cancer detection. Imaging techniques such as MRI, PET scans, and ultrasound provide detailed visualization of tumors and help guide biopsies and treatment planning. Furthermore, blood-based biomarkers and liquid biopsies offer non-invasive approaches to detect cancer-specific genetic mutations and alterations. These innovative tools hold the potential to revolutionize cancer screening and early detection, making it possible to identify cancers at their earliest and most treatable stages.
Public awareness and education about the importance of early detection and regular screening are crucial in the fight against cancer. Healthcare providers play a vital role in promoting screening guidelines and encouraging patients to undergo recommended tests. Additionally, addressing barriers to screening, such as access to healthcare and cultural stigmas, is essential to ensure that all individuals have the opportunity to benefit from early detection efforts. By prioritizing early detection and screening, we can save lives and improve outcomes for cancer patients.
Supportive Care: Managing Symptoms and Side Effects
Supportive care, also known as palliative care, is an integral part of comprehensive cancer treatment. It focuses on managing the symptoms and side effects of cancer and its treatment, improving the quality of life for patients and their families. Supportive care aims to address the physical, emotional, and psychosocial needs of patients, providing relief from pain, nausea, fatigue, and other distressing symptoms.
Pain management is a crucial aspect of supportive care, as many cancer patients experience varying degrees of pain throughout their treatment journey. Oncologists and palliative care specialists work together to develop personalized pain management plans, which may include medications, nerve blocks, and non-pharmacological approaches such as physical therapy and acupuncture. By effectively managing pain, patients can maintain their functionality and overall well-being.
In addition to pain, cancer treatment often causes a range of side effects, including nausea, vomiting, fatigue, and neuropathy. Antiemetic medications are commonly prescribed to control nausea and vomiting, while nutritional support and exercise programs can help combat fatigue. Neuropathy, a condition characterized by nerve damage, can be managed with medications, physical therapy, and lifestyle modifications. Supportive care teams work closely with patients to develop strategies for managing these side effects and improving their quality of life.
Emotional and psychosocial support is another critical component of supportive care. A cancer diagnosis can be overwhelming and emotionally challenging for patients and their families. Supportive care providers offer counseling, support groups, and mental health services to help patients cope with the emotional impact of cancer. Additionally, addressing the practical and financial aspects of cancer care, such as transportation, housing, and insurance, is essential to alleviate the burden on patients and their families. By providing comprehensive supportive care, healthcare teams can enhance the overall well-being of cancer patients and support them through their treatment journey.
The Impact of Lifestyle Choices on Cancer Prevention
Lifestyle choices play a significant role in cancer prevention, with many studies highlighting the impact of diet, physical activity, and other behaviors on cancer risk. Adopting a healthy lifestyle can reduce the likelihood of developing cancer and improve overall health and well-being. While not all cancers can be prevented, making informed choices can significantly lower the risk and promote long-term health.
Diet and nutrition are key factors in cancer prevention. A diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients and antioxidants that help protect against cancer. Conversely, a diet high in processed foods, red and processed meats, and sugary beverages has been linked to an increased risk of certain cancers, such as colorectal and breast cancer. Maintaining a healthy weight through balanced nutrition and portion control is also crucial, as obesity is a known risk factor for several types of cancer.
Regular physical activity is another important aspect of cancer prevention. Engaging in moderate to vigorous exercise for at least 150 minutes per week has been shown to reduce the risk of various cancers, including breast, colon, and endometrial cancer. Exercise helps regulate hormones, improve immune function, and maintain a healthy weight, all of which contribute to cancer prevention. Incorporating activities such as walking, running, cycling, and strength training into daily routines can have a profound impact on overall health and cancer risk reduction.
Avoiding tobacco and limiting alcohol consumption are also critical components of cancer prevention. Tobacco use is the leading cause of preventable cancer deaths worldwide, with a strong link to lung, throat, mouth, and several other cancers. Quitting smoking and avoiding secondhand smoke can significantly reduce cancer risk. Similarly, excessive alcohol consumption is associated with an increased risk of cancers such as liver, breast, and esophageal cancer. Limiting alcohol intake to moderate levels, as defined by health guidelines, can help lower the risk of alcohol-related cancers. By making conscious lifestyle choices, individuals can take proactive steps toward cancer prevention and overall well-being.
Patient Stories: Inspiring Journeys Through Cancer
The journey through cancer is often marked by resilience, courage, and hope. Patient stories provide a powerful testament to the human spirit’s ability to overcome adversity and find strength in the face of a cancer diagnosis. These stories not only inspire others but also highlight the importance of support, determination, and the advancements in cancer treatment that offer new possibilities for patients.
One such inspiring story is that of Sarah, a breast cancer survivor who was diagnosed at the age of 32. Despite the shock and fear that accompanied her diagnosis, Sarah chose to approach her treatment with unwavering determination. She underwent a combination of surgery, chemotherapy, and targeted therapy, all while maintaining a positive outlook and leaning on her support network of family and friends. Today, Sarah is cancer-free and uses her experience to advocate for early detection and support for fellow cancer patients. Her journey serves as a reminder that with the right treatment and support, it is possible to overcome even the most challenging obstacles.
Another remarkable story is that of John, a survivor of advanced melanoma. John’s cancer journey began with the discovery of a suspicious mole, which was later diagnosed as melanoma. Despite the initial prognosis, John participated in a clinical trial for an innovative immunotherapy treatment. The treatment not only halted the progression of his cancer but also led to a significant reduction in tumor size. John’s experience underscores the potential of cutting-edge therapies and the importance of clinical trials in advancing cancer treatment. Today, John continues to share his story to raise awareness about melanoma and the transformative power of immunotherapy.
These patient stories are a testament to the advancements in cancer treatment and the resilience of those who face the disease. They highlight the importance of early detection, the potential of innovative therapies, and the critical role of support systems in navigating the cancer journey. By sharing these stories, we can inspire hope, encourage others to seek timely medical care, and foster a sense of community among cancer patients and survivors.
Looking Ahead: The Future of Cancer Treatment and Research
The future of cancer treatment and research is filled with promise and potential, driven by ongoing advancements in science, technology, and medicine. As researchers continue to unravel the complexities of cancer, new avenues for treatment and prevention are emerging, offering hope for improved outcomes and ultimately, a cure for this relentless disease.
One of the most exciting areas of future research is the development of novel therapies that target specific genetic and molecular pathways in cancer cells. Advances in genomics and precision medicine are paving the way for the creation of highly targeted treatments that minimize side effects and maximize efficacy. Additionally, the exploration of combination therapies, which use multiple agents to target different aspects of cancer, holds the potential to overcome resistance and improve treatment outcomes.
Another promising frontier is the integration of artificial intelligence (AI) and machine learning in cancer research and treatment. AI algorithms can analyze vast amounts of data to identify patterns and predict treatment responses, enabling more accurate diagnosis and personalized treatment plans. Machine learning models can also assist in drug discovery, accelerating the development of new cancer therapies. The use of AI in imaging and pathology is enhancing the accuracy of cancer detection and diagnosis, leading to earlier intervention and better patient outcomes.
Furthermore, the field of cancer immunotherapy continues to evolve, with ongoing research aimed at expanding its applications and improving its effectiveness. Scientists are exploring new ways to enhance the immune system’s ability to recognize and attack cancer cells, such as developing next-generation CAR-T cell therapies and novel immune checkpoint inhibitors. The potential to harness the power of the immune system to fight cancer is one of the most promising areas of future research, offering hope for more effective and durable treatments.
As we look ahead, it is essential to continue investing in cancer research, supporting innovative clinical trials, and fostering collaboration among scientists, healthcare providers, and patients. By embracing cutting-edge science and technology, we can pave the way for a future where cancer is no longer a devastating diagnosis but a manageable and ultimately curable condition. The journey toward this future requires the collective efforts of the global community, driven by a shared commitment to improving the lives of those affected by cancer.