Esophagus cancer can be a daunting diagnosis, often leaving patients and their families grappling with fear and uncertainty. Yet, amidst the challenges, there is hope. With advancements in medical science, numerous effective treatments are now available that empower individuals to fight back against this aggressive disease. From cutting-edge surgical techniques to innovative therapies, understanding the best treatments for esophagus cancer is essential for anyone affected. This article delves deep into the most promising options that can make a significant difference in outcomes and quality of life. Whether you are navigating your own diagnosis or supporting a loved one, the journey to recovery begins with knowledge. Join us as we unveil hope and equip you with the information necessary to make informed decisions on this critical path.
Understanding Esophagus Cancer: An Overview
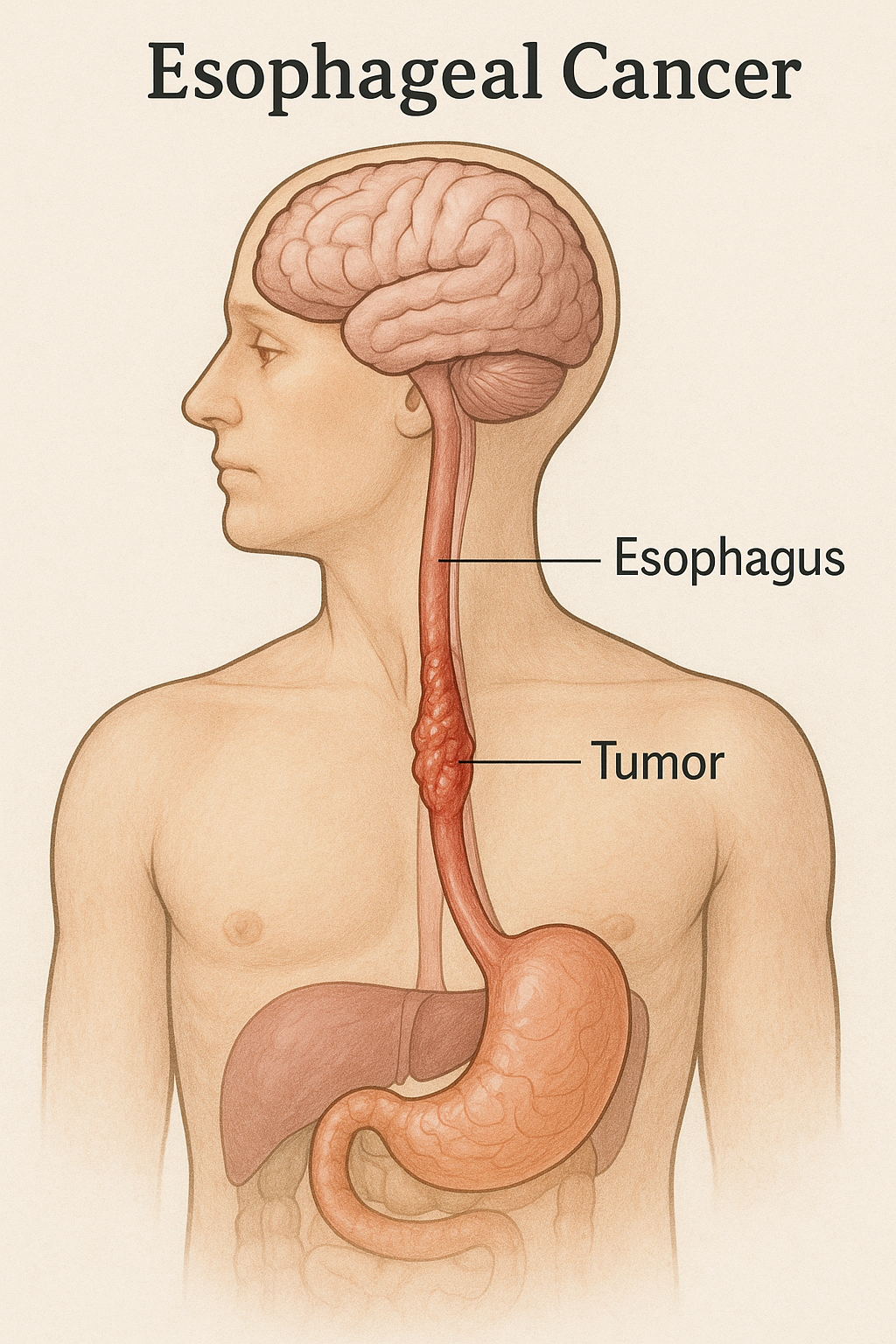
Esophagus cancer, a malignancy that originates in the esophagus—the long, hollow tube that runs from your throat to your stomach—is a formidable adversary. This cancer often begins in the cells lining the inside of the esophagus and can occur anywhere along its length. There are two main types: squamous cell carcinoma, which arises from the flat cells lining the esophagus, and adenocarcinoma, which starts in the mucus-secreting glands. The latter is more common in the lower part of the esophagus and is often associated with chronic gastroesophageal reflux disease (GERD).
While the exact causes of esophagus cancer remain somewhat elusive, several risk factors have been identified. These include smoking, heavy alcohol consumption, obesity, and a diet low in fruits and vegetables. Additionally, certain medical conditions such as Barrett’s esophagus—a precursor to adenocarcinoma—can increase the likelihood of developing this cancer. Understanding these risk factors is crucial, as it can help in early identification and prompt intervention, ultimately improving outcomes.
The global burden of esophagus cancer is significant, with high incidence rates in certain regions such as Asia and parts of Africa. Despite these statistics, advancements in medical science have paved the way for more effective treatments and improved survival rates. This article aims to shed light on these treatments, offering hope to those affected by esophagus cancer and their loved ones.
Symptoms and Diagnosis of Esophagus Cancer
Recognizing the symptoms of esophagus cancer can be challenging, as they often mimic those of less serious conditions. Early stages may present with subtle signs such as difficulty swallowing (dysphagia), which can progressively worsen as the tumor grows. Patients might also experience unintentional weight loss, chest pain, or discomfort, particularly after eating. Other symptoms include persistent coughing, hoarseness, and indigestion or heartburn that doesn’t respond to typical treatments.
Given the non-specific nature of these symptoms, a thorough diagnostic process is essential. It often begins with a detailed medical history and physical examination, followed by more specialized tests. An endoscopy, a procedure where a flexible tube with a camera is inserted down the throat, allows doctors to visually inspect the esophagus and obtain tissue samples (biopsies) for further analysis. This is a crucial step in confirming the presence of cancer cells.
Advanced imaging techniques such as computed tomography (CT) scans, positron emission tomography (PET) scans, and endoscopic ultrasound (EUS) are also employed to determine the extent of the disease. These imaging modalities provide detailed information about the size and spread of the tumor, which is vital for staging the cancer and planning the appropriate treatment strategy. Early and accurate diagnosis is paramount, as it significantly influences the chances of successful treatment and recovery.
Staging of Esophagus Cancer: What You Need to Know
Staging is a critical aspect of esophagus cancer diagnosis, as it helps determine the extent of the disease and guides treatment decisions. The staging system commonly used is the TNM system, which stands for Tumor, Node, and Metastasis. This system assesses the size and spread of the primary tumor (T), the involvement of nearby lymph nodes (N), and the presence of distant metastasis (M).
Stage 0, or carcinoma in situ, indicates that the cancer is confined to the innermost layer of the esophagus and has not spread. Stage I cancer is limited to the esophagus but has penetrated deeper layers. Stage II involves the spread to nearby lymph nodes or the outer layers of the esophagus. Stage III signifies more extensive spread to surrounding tissues or more lymph nodes. Finally, Stage IV indicates that the cancer has metastasized to distant organs, such as the liver or lungs.
Accurate staging is achieved through a combination of diagnostic tests, including endoscopic ultrasound, CT scans, PET scans, and sometimes laparoscopy. This meticulous process ensures that the chosen treatment plan is tailored to the specific stage and characteristics of the cancer, maximizing the chances of a positive outcome. Understanding the staging process empowers patients and their families with the knowledge needed to navigate their treatment journey effectively.
Surgical Options for Esophagus Cancer Treatment
Surgery plays a pivotal role in the treatment of esophagus cancer, particularly for those diagnosed at an early stage. The primary goal of surgery is to remove the tumor and a margin of healthy tissue, which can potentially cure the disease. The type of surgery depends on the location and stage of the cancer, as well as the patient’s overall health and preferences.
Esophagectomy, the most common surgical procedure for esophagus cancer, involves the removal of a portion of the esophagus and, in some cases, part of the stomach. The remaining esophagus is then reconnected to the stomach to allow for normal swallowing and digestion. There are different approaches to esophagectomy, including the transthoracic approach (through the chest), the transhiatal approach (through the abdomen and neck), and minimally invasive techniques that use smaller incisions and specialized instruments.
In some instances, endoscopic procedures may be an option for very early-stage cancers. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) involve the removal of superficial tumors through an endoscope, offering a less invasive alternative to traditional surgery. These procedures are often followed by additional treatments, such as radiation or chemotherapy, to address any remaining cancer cells and reduce the risk of recurrence.
Surgical interventions for esophagus cancer are complex and require the expertise of a multidisciplinary team, including surgeons, oncologists, and gastroenterologists. Postoperative care and monitoring are crucial to ensure proper healing and address any complications. While surgery can be demanding both physically and emotionally, it remains one of the most effective treatments for achieving long-term remission and improving survival rates.
Radiation Therapy: How It Works and Its Benefits
Radiation therapy is a cornerstone in the treatment of esophagus cancer, often used in conjunction with surgery or as a standalone therapy for patients who cannot undergo surgery. This treatment employs high-energy beams, such as X-rays or protons, to target and destroy cancer cells. The precision of radiation therapy allows for the concentration of doses on the tumor while minimizing damage to surrounding healthy tissues.
There are two main types of radiation therapy used for esophagus cancer: external beam radiation therapy (EBRT) and brachytherapy. EBRT involves directing radiation beams from outside the body towards the tumor, typically over several weeks. Brachytherapy, on the other hand, involves placing radioactive material directly inside or near the tumor, providing a high dose of radiation to the cancerous cells while sparing adjacent tissues. This method is often used for localized tumors or to relieve symptoms in advanced cases.
The benefits of radiation therapy are multifaceted. It can shrink tumors before surgery, making them easier to remove, or it can be used postoperatively to eliminate residual cancer cells and reduce the risk of recurrence. For patients with advanced or inoperable esophagus cancer, radiation therapy can offer palliative relief, alleviating symptoms such as pain, bleeding, or difficulty swallowing. Advances in technology, such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), have further enhanced the precision and effectiveness of this treatment, leading to better outcomes and fewer side effects.
Despite its advantages, radiation therapy is not without challenges. Patients may experience side effects, including fatigue, skin reactions, and irritation of the esophagus, which can cause pain or difficulty swallowing. However, these side effects are generally manageable and temporary. A comprehensive treatment plan, developed by a team of specialists, ensures that the benefits of radiation therapy outweigh the risks, offering patients a valuable tool in their fight against esophagus cancer.
Chemotherapy: Types and Effectiveness
Chemotherapy, a systemic treatment that uses drugs to kill cancer cells, is a mainstay in the management of esophagus cancer. It can be administered before surgery (neoadjuvant chemotherapy) to shrink tumors, making them easier to remove, or after surgery (adjuvant chemotherapy) to target any remaining cancer cells and reduce the likelihood of recurrence. In cases where surgery is not an option, chemotherapy can be combined with radiation therapy (chemoradiation) to improve outcomes.
There are several types of chemotherapy drugs used to treat esophagus cancer, often in combination to enhance their effectiveness. Commonly used agents include cisplatin, fluorouracil (5-FU), carboplatin, and paclitaxel. These drugs work by interfering with the cancer cells’ ability to grow and divide, ultimately leading to their death. The choice of drugs and the specific regimen depend on factors such as the stage of the cancer, the patient’s overall health, and previous treatments.
The effectiveness of chemotherapy varies, with some patients experiencing significant tumor shrinkage and prolonged survival, while others may have more modest responses. Nevertheless, chemotherapy remains a critical component of a comprehensive treatment strategy, particularly for advanced-stage esophagus cancer. It can also help alleviate symptoms and improve quality of life for patients with metastatic disease.
While chemotherapy can be highly effective, it is associated with a range of side effects due to its impact on rapidly dividing cells, both cancerous and healthy. Common side effects include nausea, vomiting, hair loss, fatigue, and increased susceptibility to infections. Advances in supportive care, such as anti-nausea medications and growth factors, have improved the management of these side effects, enabling patients to better tolerate treatment. The development of new chemotherapy agents and combination therapies continues to enhance the effectiveness and tolerability of this treatment, offering hope to those battling esophagus cancer.
Targeted Therapy: A New Frontier in Treatment
Targeted therapy represents a significant advancement in the treatment of esophagus cancer, offering a more precise approach to attacking cancer cells. Unlike traditional chemotherapy, which affects all rapidly dividing cells, targeted therapy specifically targets molecules involved in the growth and survival of cancer cells. This precision reduces damage to healthy cells and minimizes side effects, making targeted therapy an attractive option for many patients.
One of the key targets in esophagus cancer therapy is the HER2 protein, which is overexpressed in a subset of esophageal adenocarcinomas. Trastuzumab (Herceptin) is a monoclonal antibody that targets HER2 and has shown significant benefits when combined with chemotherapy. Another promising agent is ramucirumab, an anti-angiogenesis drug that inhibits the formation of new blood vessels needed by tumors to grow and spread. These targeted therapies have demonstrated improved response rates and survival outcomes in clinical trials.
The development of targeted therapies is driven by a deeper understanding of the molecular and genetic underpinnings of esophagus cancer. Researchers are continually identifying new targets and developing drugs to exploit these vulnerabilities. For example, inhibitors of the epidermal growth factor receptor (EGFR) and MET signaling pathways are being investigated for their potential to treat esophagus cancer. The advent of biomarker testing allows for the identification of patients who are most likely to benefit from these therapies, personalizing treatment and improving outcomes.
The integration of targeted therapy into the treatment landscape of esophagus cancer represents a paradigm shift, offering hope to patients with advanced or resistant disease. As research progresses, the portfolio of targeted therapies is expected to expand, providing more options and improved prognosis for those affected by this challenging cancer.
Immunotherapy: Harnessing the Body’s Defense Mechanism
Immunotherapy has emerged as a groundbreaking approach in the fight against esophagus cancer, leveraging the body’s immune system to recognize and destroy cancer cells. This innovative treatment modality has shown remarkable success in various cancers, and its application in esophagus cancer is rapidly evolving. Immunotherapy works by enhancing the immune system’s ability to detect and attack cancer cells, which often evade immune surveillance through various mechanisms.
One of the most promising forms of immunotherapy is the use of immune checkpoint inhibitors. These drugs, such as pembrolizumab (Keytruda) and nivolumab (Opdivo), block proteins that inhibit immune responses, thereby unleashing the immune system to target cancer cells. Clinical trials have demonstrated significant benefits of these inhibitors in patients with advanced or metastatic esophagus cancer, particularly those with tumors expressing high levels of PD-L1, a protein that helps cancer cells escape immune attack.
In addition to checkpoint inhibitors, other immunotherapeutic approaches are being explored, including cancer vaccines and adoptive cell therapy. Cancer vaccines aim to stimulate the immune system to recognize and attack specific cancer antigens, while adoptive cell therapy involves the infusion of immune cells that have been engineered or expanded to enhance their cancer-fighting capabilities. These innovative strategies hold great promise and are the focus of ongoing research and clinical trials.
The integration of immunotherapy into the treatment paradigm for esophagus cancer represents a significant advancement, offering new hope for patients with limited options. While not all patients respond to immunotherapy, those who do can experience durable responses and improved survival. The ongoing research and development in this field are expected to further refine and expand the use of immunotherapy, providing more effective and personalized treatment options for esophagus cancer.
Lifestyle Changes and Supportive Care for Patients
In addition to medical treatments, lifestyle changes and supportive care play a crucial role in the overall management of esophagus cancer. These measures can help alleviate symptoms, improve quality of life, and enhance the effectiveness of treatment. Adopting a healthy diet, staying physically active, and avoiding tobacco and excessive alcohol consumption are some of the key lifestyle changes that can positively impact patients’ health and well-being.
Nutrition is particularly important for patients with esophagus cancer, as the disease and its treatments can cause difficulties with swallowing and digestion. A dietitian can provide personalized dietary recommendations to ensure adequate nutrition and prevent weight loss. Soft, high-calorie, and nutrient-dense foods are often recommended, along with strategies to manage swallowing difficulties. In some cases, enteral nutrition through a feeding tube may be necessary to maintain nutritional status during treatment.
Supportive care, also known as palliative care, focuses on relieving symptoms and improving the quality of life for patients at any stage of esophagus cancer. This care is provided by a multidisciplinary team that includes doctors, nurses, social workers, and other specialists. Pain management, nutritional support, psychological counseling, and spiritual care are some of the components of supportive care. These services help address the physical, emotional, and social challenges associated with esophagus cancer, providing comprehensive support to patients and their families.
Engaging in regular physical activity, as tolerated, can also benefit patients by improving overall fitness, reducing fatigue, and enhancing mood. Gentle exercises such as walking, yoga, and stretching can be tailored to individual capabilities and preferences. Additionally, staying connected with a support network, whether through family, friends, or support groups, can provide emotional strength and encouragement during the cancer journey.
Overall, lifestyle changes and supportive care are integral to the holistic management of esophagus cancer, complementing medical treatments and helping patients navigate the challenges of the disease. By addressing the physical, emotional, and social aspects of care, these interventions contribute to a better quality of life and improved outcomes for patients.
Conclusion: Hope and Future Directions in Esophagus Cancer Treatment
The landscape of esophagus cancer treatment has evolved significantly, offering new hope to patients and their families. From advanced surgical techniques to innovative therapies such as targeted therapy and immunotherapy, the arsenal of treatments available today provides a multifaceted approach to tackling this aggressive disease. Each treatment modality, whether used alone or in combination, plays a crucial role in improving survival rates and enhancing the quality of life for patients.
The future of esophagus cancer treatment looks promising, with ongoing research and clinical trials poised to uncover new strategies and therapies. The continued exploration of molecular and genetic underpinnings of the disease will likely lead to more personalized and effective treatments. The integration of cutting-edge technologies, such as artificial intelligence and precision medicine, holds the potential to revolutionize cancer care, offering tailored interventions based on individual patient profiles.
Moreover, the emphasis on early detection and prevention cannot be overstated. Public awareness campaigns, routine screenings for high-risk individuals, and lifestyle modifications are essential components of a comprehensive approach to reducing the incidence and improving outcomes of esophagus cancer. By fostering a proactive mindset and encouraging healthy behaviors, we can make strides in the fight against this challenging disease.
In conclusion, while esophagus cancer remains a formidable diagnosis, the advancements in treatment and supportive care offer a beacon of hope. Armed with knowledge and empowered by the latest medical innovations, patients and their families can navigate the journey with confidence and optimism. The collective efforts of researchers, healthcare professionals, and the broader community continue to drive progress, paving the way for a brighter future in esophagus cancer treatment.